Authors / metadata
DOI: 10.36205/trocar6.2025020
Abstract
Deep Infiltrating Endometriosis (DE) is a multifaceted gynaecological disorder that requires the integration of different disciplines. This review focuses on the Multidisciplinary Team (MDT) approach in the care and management of DE, highlights the key considerations, and explores future implications. An MDT, generally involving gynaecologists, colorectal surgeons, urologists, and pain specialists directed towards more accurate diagnosis, improved surgical outcomes and greater patient-centred symptom management. The potential barriers to MDT include financial and logistical restraints, issues related to seamless coordination between multiple disciplines, and unintentional treatment delays. Strategies to overcome these barriers must include standardizing care processes, capitalizing on developments in tele-conferencing, aligning patient pathways to avoid duplication of service and putting services in place that would be responsive to patient needs by engaging patients in patient-centred research. Although clear barriers exist, the MDT approach should provide benefits in the management of DE. The MDT approach engages closely with recommendations from leading organizations and should apply principles that are fundamental to optimal service delivery of health care. It is necessary to address these barriers to attain holistic care and management of DE.
Abbreviations: MDT- Multidisciplinary team, VATS – Video-Assisted Thoracoscopic Surgery, DE – Deep Infiltrating Endometriosis
Introduction
Endometriosis is an increasingly common gynecological disease that affects a significant proportion of reproductive-age women throughout the world. Endometriosis involves the presence of endometrial glands and stroma outside of the uterus with a number of different presentations, including peritoneal endometriosis, ovarian endometriosis, and DE (1–3). DE is an aggressive form of endometriosis that invades greater than 5 mm below the peritoneal surface. The presence of DE can affect multiple organ systems including the bowel, urinary tract, as well as distant invasions to the thoracic cavity (the lungs and diaphragm). Bowel endometriosis has a significant prevalence in the population of women with pelvic endometriosis (5-40%) and up to 10% of these women have urinary tract endometriosis (3). The complexity of DE involves numerous systems, therein making definitive treatment challenging: thus, a comprehensive and multidimensional global approach in management is important. In fact, there has been a better appreciation recently for the MDT approach to manage the difficulties of DE. The MDT approach to management certainly indicates a shift in the direction of optimal healthcare (4). For example, the 1995 the Calman-Hine report suggested MDT approach to chronic disease management was the best model (5). Additionally, the European Society for Human Reproduction and Embryology (ESHRE) Guidelines on the Diagnosis and Management of Endometriosis highlighted that the MDT approach should be the “gold standard” for the management of complex clinically significant cases of DE (6). The guidelines emphasize the importance of referring patients to tertiary centres with the necessary expertise providing the treatments are offered in a multidisciplinary context (6). The British Society for Gynaecological Endoscopy, (BSGE) recently put forward criteria for organizations undertaking complex endometriosis surgical procedures, which acknowledge the importance of a multidisciplinary team including colorectal surgeons and nurse specialists (3,7,8). The MDT approach provides integrated care that accounts for the multidimensional aspects of DE. These aspects ensure accurate diagnosis, surgical planning and holistic care with psychological input (9-18). However, we must consider and address potential obstacles and limitations to implementing this approach. This opinion paper investigates the role of the MDT in the management of DE, including its potential benefits and obstacles that need to be addressed to optimize outcomes for women with DE.
Material and Methods
This is an opinion paper informed by more than 15 years of clinical experience with an evidence-based support. A literature search was undertaken in the scientific databases managed by PubMed, Springer Nature, and Elsevier for literature research in English from 2010 to 2024. Varying combinations of the relevant terms were used: “multidisciplinary-team,” “multidisciplinary-approach,” “multidisciplinary-care,” “multidisciplinary-treatment,” “deep-infiltrating endometriosis.” All relevant articles were examined including references, and thirty-three relevant papers have been included in this paper. A retrospective review of the case of a 41-year-old nulliparous female with clinically severe DE, who was managed by an MDT approach, was also included. The case highlights the potential benefit of an interdisciplinary approach with respect to surgical planning, intraoperative management and postoperative care.
A Multidisciplinary Team (MDT) Approach- WHAT does this mean?
A multidisciplinary team approach is a collaborative model of healthcare that integrates professionals from diverse disciplines to provide comprehensive coordinated care for patients with complex medical conditions (3,4,7). The MDT approach has significantly gained recognition and has been implemented across various medical fields, especially in managing chronic and multifaceted diseases. The MDT approach has increasingly become significant in managing endometriosis due to the disease’s complexity and its broad impacts on the lives of patients (11). The MDT usually comprises gynaecologists, colorectal surgeons, urologists, radiologists, cardiothoracic surgeons, pain management specialists/anaesthesiologists, fertility experts, physiotherapists, specialized nurses, nutritionists, and psychologists (3,19). The core of the MDT approach involves regular team meetings focused on discussing patient cases and formulating treatment plans. The forums ensure shared decision-making where each individual contributes their expertise to develop a comprehensive approach to managing the patient’s condition. This ensures that all aspects of the patient’s care are considered from the onset, diagnostic procedures to surgical planning and long-term care in management including psychological support (3).
Rationale for MDT Approach in DE – The “WHY”
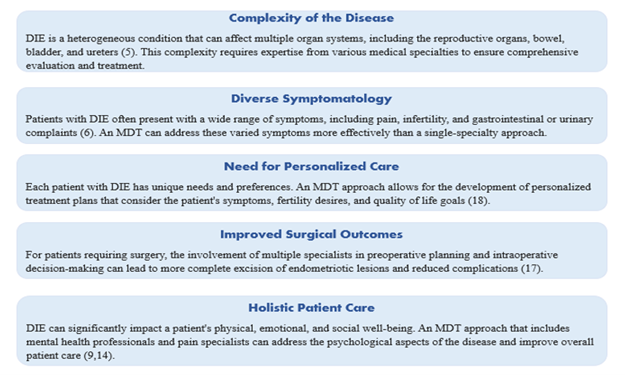
Perspective underscores the importance of an MDT approach in managing DE: Authors’ Illustration of the rationale for MDT in DIE (Fig 1). Implementing the MDT approach to managing DE offers potential benefits including:
Improved diagnostic accuracy: The MDT approach combines the expertise of various specialists, allowing for a more comprehensive and quicker evaluation of the patient’s condition (3,18).
Better surgical outcomes: The MDT approach provides a collaborative platform yielding better surgical outcomes such as fertility preservation and reduced pain. It reduces complication rates and ensures more complete excision of endometriotic lesions whilst ensuring conservation of function (17,18).
The MDT approach provides effective pain management strategies.: Pain specialists and physiotherapists within the MDT integrate pharmacological and non-pharmacological modalities to address the chronic pain associated with DE (15,17). The MDT approach ensures a more efficient use of healthcare resources, averting fragmented care and redundant interventions. It provides a collaborative environment that facilitates opportunities for research and innovation in treating DE, advancing clinical practice as well as the scientific understanding of the disease (20,21).
Enhanced fertility management: An MDT involving fertility specialists can optimize the timing and type of treatments including pre-operative harvesting and freezing of ova to avert risks of loss of ovarian reserve that occurs with surgery.
Psychological support: Given the emotional toll of chronic illness, access to psychological support within the MDT can improve a patient’s mental health and overall quality of life, reducing risks and burden of anxiety or depression, typical with endometriosis.
Cost-effectiveness: Currently, most endometriosis patients must undergo repeated visits, evaluations, treatments, or surgeries. In an MDT approach, there is optimal care right from early diagnosis to better surgical and medical outcomes with treatment planning that minimizes patient risk.
Continuity of care: Coordinated care allows smoother transitions between different treatments and follow-up appointments, improving overall DIE management and ensures patient satisfaction.
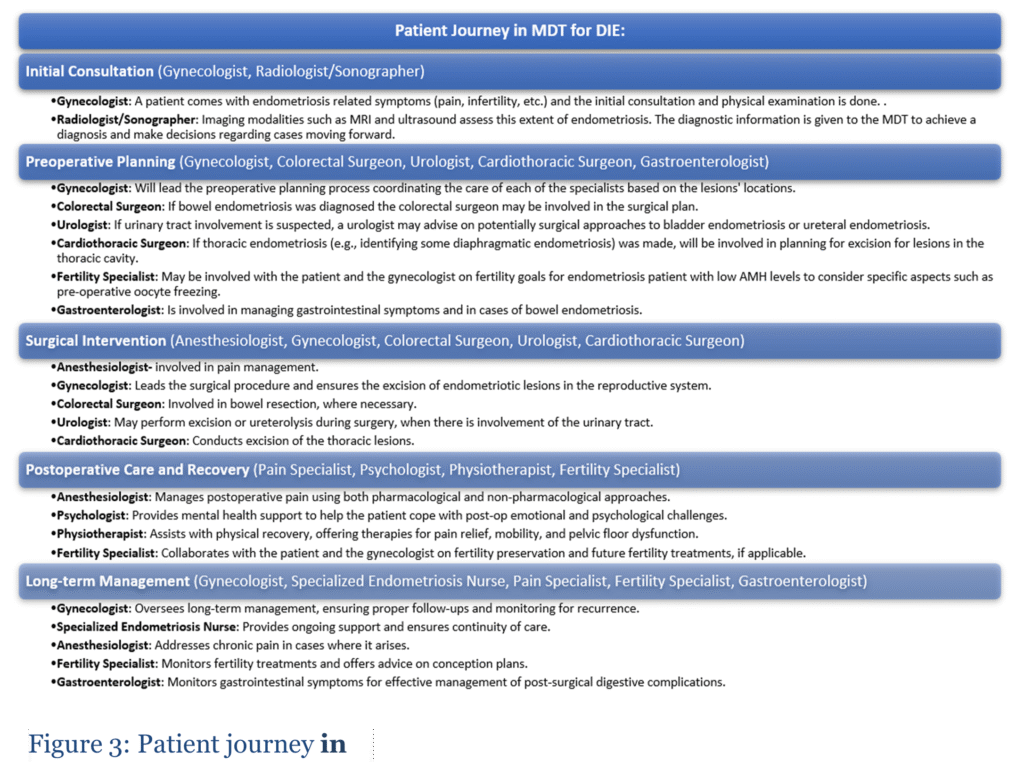
Elements of an MDT for Endometriosis: What makes up an MDT is illustrated in Figure 2. The gynaecologist, with special interest in endometriosis, is typically the main team member responsible for managing the gynecological aspects of care for the patient. This would include an initial assessment of the patient, the surgical management of the gynaecological aspects of endometriosis, and the overall management of the treatment plan for the patient. As a specialized clinician, the gynaecologist plans and completes complex laparoscopic surgeries for endometriosis excision (3,22,23). He/she collaborates with the radiologist/sonographer in the patient assessment process to obtain the diagnostic imaging assessment of the extent and location of DE. Accurate imaging is essential for optimal operative planning as well as postoperative assessments and evaluation (24). The colorectal surgeon has a vital role when there is bowel involvement requiring surgery. Depending on the size, extent, and location of the nodule, the colorectal surgeon will advise on the type of surgery to be performed and conduct the procedure alongside the gynecologist (3,16,20,25). Urologists play a critical role when endometriosis involves the urinary tract (mostly the bladder and ureters). They may be part of the patient’s preoperative evaluation to determine the extent of disease involvement (26). During surgery, they may collaborate with the gynecologist to excise bladder and ureteral endometriosis using the best surgical approach (26). A cardiothoracic surgeon is crucial in cases involving thoracic endometriosis (27,28). Surgical intervention may include the excision of thoracic or diaphragmatic endometriotic lesions (27). Pain management is a critical aspect of endometriosis care. Pain specialists/anaesthesiologists provide better approaches and strategies (both pharmacological and non-pharmacological) for chronic pain management (12,21,29,30). Infertility is often one of the primary symptoms of endometriosis in women of reproductive age. Fertility specialists are commonly a part of the MDT as they can provide input on fertility preservation and on the timing of fertility treatment with other management goals for endometriosis (6,31,32). Women with endometriosis frequently describe having gastrointestinal symptoms, including bloating, dyschezia and constipation. Treating endometriosis improves these symptoms. Occasionally, the patient may require a referral to a gastroenterologist for consultation. The gastroenterologist will identify the cause of the gastrointestinal symptoms (e.g., gastrointestinal bleeding), providing an accurate diagnosis and management of gastrointestinal complications related to endometriosis (20). Often, the specialized endometriosis nurse will be resourceful to patients given that they are the care coordinator. They create continuity of care and connection with the patient and team (22). The physiotherapist addresses the musculoskeletal challenges frequently associated with endometriosis and pelvic floor dysfunction. Physiotherapists assist with treatment to alleviate associated pain, pelvic floor function, and general feeling of physical wellness (2,15). Endometriosis has significant psychological impacts. Patients can experience depression and anxiety, relationships, and self-esteem issues. Psychologists are crucial in the MDT. They walk with patients in their journey toward their optimal mental health (10,11,14). The Gynaecologist is at the core of coordinating the various specialties in providing care at various stages in endometriosis management (Figure 2).
A Typical Care Journey of an Endometriosis patient:
In a typical care journey, a patient may first present to a physician with the typical symptoms and other cyclical pain experiences such as chest pain and low back pain. In these situations, symptoms can be misattributed to other issues, physicians refer to different specialists inconsistently, leading to a delayed diagnosis and disrupted care. The initial consultation occurs before diagnosis. A patient is typically diagnosed after a consultation when imaging (ultrasound or MRI) has been requested and carried out, and after sending a referral for a diagnostic laparoscopy. Once a treatment plan is established and surgery is booked, it is common for a patient to be referred to one specialist, usually a gynecologist, who will make all decisions regarding their care, without collaboration or collegiality from other specialists that may have been involved, such as colorectal surgeons, urologists, etc. In seeking postsurgical care, often, the patient experience is singularly concerned with the resolution of their symptoms, usually without holistic recovery, as there was minimal support for the emotional, psychological, and fertility issues that patients have. Patients talk about receiving good care from their specialists, highlighting concerns regarding the issues surrounding re-emergence of symptoms. For true longitudinal care of this chronic condition, there is insufficient collaboration or collegiality amongst specialists. However, an MDT approach is a completely different experience, as we have intentionally designed and integrated collaborative models of input from different specialists (Figure 3).
Navigating the Potential Challenges/Barriers
While there are significant benefits to MDT, there are also some critical challenges and barriers that must be addressed. The MDT model engages various specialties in patient care. Its coordination, if not seamless, can severely impact the success of the MDT model of care. Developing written or well-orchestrated communication systems and decision pathways is necessary to address such challenges (4,33). The MDT model requires significant resources. Involving MDTs for DE management will be a challenge in some care settings such as in rural/remote healthcare. There will be fewer or no specialists, as the access to higher specialty care is more limited in their areas. This disparity creates many challenges to providing the best possible DE care in the most complex cases. It will be necessary to discuss and examine alternative and cost-effective models of care for implementing MDT principles across the health care continuum (4).
Consultation delay:
Could occur because an MDT assessment implies consulting multiple specialties. A thorough assessment is the clear priority consideration, but must be managed adequately against time. As such, all specialists must jointly facilitate referral consultations and to ensure that there are correct treatment pathways for the patients to follow to mitigate treatment delay (4). Differences in MDT composition and practices across health care settings may lead to variability in DE care. It is important to develop standardized protocols for the MDT approach regardless of health care setting. New approaches such as virtual MDT meetings may be important for addressing challenges related to geographical distance and service access for specialized services for patients in remote areas, which is to be appreciated. This will assist the MDT in effectively optimizing care for patients with DE and improving patient outcomes (4).
Endometriosis Case Study Demonstrating the MDT Approach
The case involves a 41-year-old nulliparous woman, with a history of right groin pain, menorrhagia and dysmenorrhea. A detailed transvaginal ultrasound scan for DE was performed by the radiologist. The findings revealed a uterus with extensive diffuse adenomyosis, multiple small intramural myomas, with a negative sliding sign both anteriorly and posteriorly. Extensive endometriosis was noted: Bilateral uterosacral ligaments nodules, the right measuring 2.7 cm x 0.9 cm and the left measuring 1.6 cm x 0.83 cm, Torus nodules (3.0 cm x 0.6 cm and 3.8 cm x 1.0 cm), Bowel nodule with significant deep infiltration, tubo-ovarian pelvic adhesions, and inguinal avascular nodule (3.2 cm x 2.0 cm) about 2 mm away from femoral artery. A pseudo-cyst involving the bladder was also noted. The #Enzian classification for the ultrasound findings was: T2/2, A3, B2/2, C3, FA, FB, F(inguinal) + Myoma.
The following observations were made during surgery:
- The uterus was adherent to the anterior abdominal wall and bladder.
- Bilateral fallopian tubes were adherent to the uterus, ovaries, lateral pelvic wall, and bowel.
- Thickening of the pelvic peritoneum was noted near the left external iliac vein.
- Bilateral uterosacral ligaments displayed thickening with endometriotic and torus nodules.
- A right hydro-ureter was observed due to compression by an endometriotic nodule.
The Intra-operative findings had the following #Enzian classification: P3, T3/3, A3, B3/3, FA, FB, F(inguinal) + Myoma. Laparoscopic surgery for endometriosis (lasting 7 hours and 16 minutes) involved the following key areas – demonstrating the MDT approach the anaesthetist did administer regional blocks and analgesics. The gynaecologist performed the following:
- Bilateral ureterolysis
- Endometriotic nodules resection from the bilateral uterosacral ligaments and torus.
- Freeing of the bowel from adhesions to the uterus, right ovary, and lateral pelvic wall.
- Resection of an endometriotic nodule from the right lateral pelvic wall near the external iliac vein (peritonectomy).
- Detaching the uterus from the anterior abdominal wall and bladder.
- A right salpingectomy.
The colorectal surgeon performed the following:
- Rectal mobilization and nodule shaving
- Ileocecal resection and appendicectomy using a linear stapler.
- Rectal nodule resection.
A vascular and general surgeon:
- collaborated on the right iliac fossa nodule resection (laparotomy) and subsequent mesh repair, as the nodule extended towards the thigh.
Post-Op Follow-up:
Outcome and progress pain management: the patient reports reduced pain and indicates improved quality of life. Nutritional support: specialized nutritional advice was provided on anti-inflammatory foods and gut health after major bowel surgery. A structured meal plan was introduced to complement wound repair and reduce post-operative inflammation. It was recommended that small, frequent meals be attempted during the early recovery period, with transition to a regular diet as soon as bowel function returns to normal. Physiotherapy: the patient was seen by the physiotherapist for mobilization of the pelvic floor muscles. Psychological support: the patient was linked to a clinical psychologist with specialized knowledge in chronic pain and fertility concerns. Regular counselling was done regarding the surgery, pain control, and fertility issues. The psychological support helped develop coping strategies for possible anxiety and depression that could arise out of the long recovery process. The patient is currently on suppression therapy awaiting fertility treatment.
Conclusion
The MDT model is regarded as a key evolution in managing DE and an advancement toward the more holistic and patient-centred care. The MDT brings together clinicians from various specialties, including obstetricians and gynaecologists, colorectal surgeons, urologists, radiologists, chronic pain experts, fertility experts, and psychologists to ensure each perspective relating to a patient’s presentation has been modelled into the individualized care. The MDT is a collaborative effort for which clinicians contribute their specialties over time, with prospectives for future innovation for managing DE effectively. The key challenges associated with an MDT approach include limited resource base, scheduling and coordinating the various specialists, unequal access to these specialists and resources, resulting in potential delays in DE management. These issues suggest variations in quality of care. There is a need for standardized practices whilst accommodating local needs and resources. Knowledge education is necessary to enhance standard of care. Therefore, an MDT approach has great potential to manage DE, but potential barriers must be addressed to create an opportunity to work towards true patient-centred, holistic and effective care for this complex condition.