Authors / metadata
DOI: 10.36205/trocar6.2025022
Abstract
Leiomyoma of the vulva are very uncommon entities and account for only 0.03% of all gynecological tumours and 0.07% of vulvar tumours in women (1). These mainly occur in women of childbearing age. The patient presented here is 36-year-old women who had found a painless vulvar mass measuring 3x4x3cm at the level of the posterior vaginal opening that was misdiagnosed as a Bartholin’s cyst when she was admitted to the hospital, but it turned out to a vulvar leiomyoma during surgery, which was also confirmed by pathology.
Introduction
A leiomyoma of the vulva was first reported by Denys de Leyden in 1733, and its etiology is still unclear. It is generally believed that estrogen and progesterone may contribute to tumor proliferation, as seen with fibroids, which rarely occurs before menarche and usually shrinks or resolve after menopause. A vulvar leiomyoma is very rare benign tumour originating from the smooth muscle cells of the vulvar tissue. It usually grows in the vicinity of the Bartholin ‘s gland, and can also be seen in the labia majora, labia minora, and clitoris. It presents mostly as a unilateral oval mass, with good mobility, moderate texture, no tenderness, with an independent capsule, and clear boundary with the surrounding tissues. Patients often present with a mass in the vulva, generally without discomfort, a very small number of patients experience pain, erythema, and itching over the lesion site. The maximum diameter of a leiomyoma in the vulva can reach up to 10 cm, accompanied by symptoms such as heaviness in the vulva, discomfort during sexual intercourse, difficult walking, and it can also present as a pedunculated mass on the vulvar epithelium (2).
Case presentation
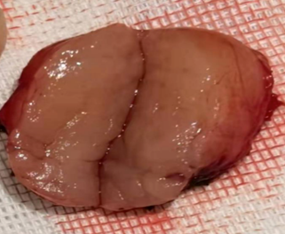
The patient is a 36-year-old female who had discovered a mass in the vulva for four years that gradually enlarged over the last year. She had one natural delivery and an episiotomy to the left, without any other history of vulvar surgery. At first the size of the mass was about the size of a peanut kernel, and she did not pay much attention to it, the vulvar mass gradually increased in size over the past year and was slightly tender on light pressure. The patient visited our gynecological clinic last year, and the physical examination showed a mass of about 3x4x3 cm in size located in the posterior region of the vaginal opening, with moderate consistency, clear boundaries, and good mobility, without obvious tenderness. The patient was admitted to the hospital with a diagnosis of right Bartholin ‘s cyst. Excision of vulvar lesion was performed after preoperative examinations. The mass was located beneath the fat layer and had clear boundaries with the surrounding tissues. Pathology result confirms the mass to be a leiomyoma of the vulva. (Figure 1, 2). The patient was followed up for one year after the operation. There was no recurrence nor any complaints.
Discussion
Clinically is very easy to misdiagnose a leiomyoma of the vulva as a Bartholin’s cyst (abscess). The latter is an enlarged mass that can be seen in the lateral part of the vestibule of the vagina on the affected side at pelvic examination, and presents as a cystic mass with fluctuation that can be palpated in the posterior inferior part of the vulva. A vulvar leiomyoma can grow in any part of the vulva, with moderate consistency but is of a solid consistence without fluctuation. In addition, it is still necessary to differentiate from diseases such as sebaceous cyst of vulva, lipoma, fibroma, schwannoma, angiomyofibroblastoma (3). The preoperative diagnosis of vulvar masses can be clinical but can also include imaging. Magnetic resonance imaging (MRI) may have a beneficial role in diagnosing vulvar leiomyoma because of the low signal intensity suggesting smooth muscle on T2-weighted images. It would be advisable to perform a trans labial ultrasound with a transvaginal probe or even better with a high-frequency linear probe before performing an MRI, the latter being expensive and time-consuming. Trans labial ultrasound provides a more precise differential diagnosis: Bartholin’s gland, a dense, densely packed fluid or fluid mass with exclusively peripheral vascularization, vulvar fibroma, a solid mass with likely both central and peripheral vascularization. The final diagnosis depends on the postoperative pathologic report and immunohistochemistry microscopically, the pathological patterns are similar to those of a uterine leiomyoma, with spindle cells arranged in bundles or whorls. For tumors with a diameter of > 5 cm, unclear boundaries, > 5 mitoses /10 HP, and significant atypical hyperplasia of cells, the possibility of vulvar leiomyosarcoma should be considered (4). Immunohistochemical markers such as SMA, desmin, and vimentin can assist in diagnosis, and some may show ER (+), PR (+).
The vulvar leiomyoma should be treated actively once diagnosed, and surgical resection with pathological diagnosis should be performed to exclude the possibility of a malignant tumor of vulva, tumor tissue should be completely resected because of the possible recurrence, and a long-term follow-up should be performed after the operation. It has been reported that the time of postoperative recurrences can be as long as more than ten years (5). There are reports of vulvar leiomyoma in pregnancy with rapid growth of the mass during gestation, considered to be related to elevated estrogen and progesterone levels (6). For pregnant patients presenting with a vulvar leiomyoma, the nature and size of the tumor, gestational weeks, whether the birth canal is obstructed, the risk of surgical bleeding and infection, and the risk of abortion and premature delivery should be considered comprehensively, and then a reasonable treatment plan should be formulated (7).
Conclusion
In conclusion, due to the rarity of the vulvar leiomyoma and its tendency to be misdiagnosed, it is necessary to perform imaging examination preoperatively such as ultrasound scan or MRI, trans labial ultrasound should be given priority as it is convenient and inexpensive, regardless of the clinical experience of the surgeon.
Acknowledgment: The authors thank Bruno J van Herendael for his positive criticism and help during the writing.